Course Info
Daily Value
| Type | 100% DV | Goal |
|---|---|---|
| total fat | 78g | less than |
| sat. fat | 20g | less than |
| sodium | 2300mg | less than |
| total carb | 275g | at least |
| dietary fiber | 28g | at least |
| added sugar | 50g | less than |
| protein | 50g | at least |
Nutrient DV and food source
- A food that provides >20% DV is considered high in that nutrient.
- A food that provides DV of 10-19% is considered a good source for that nutrient.
- A food that provides <5% is a low source of that nutrient.
Intro to nutrition
notes from 4/3/23
Is breakfast the most important meal of the day? No
- regular meal prevents being overly hungry
- breakfast is not necessarily the most important meal of the day
- breakfast is a loose concept (the meal the breaks the nighttime fast)
- as long as you don’t feel fatigue or extremely tired, it’s not necessary to eat breakfast
Is calorie count important?
- follow the food matrix, not just the calorie content
factors of food choice:
- taste (top factor)
- price
- culture / socially appropriateness
- mood / stress level
- knowledge about nutrition
- accessibility
don’t pay too much attention to social media for food choice
- what people post may not actually be what they eat
- just because a diet works for someone doesn’t mean it works for you
what makes a diet healthy?
food eaten per year: 1,000,000 kcal per year = 1,500 lbs per year
body renews itself:
- blood
- hair
- skin (shedding → dust)
- intestine
macronutrients
- protein
- carbohydrate
- fat
- water (no energy)
micronutrient
- minerals
- vitamins
male has more muscles, female hsa more body fat (to sustain pregnancies) 55-60% water 15-25% fat 18-20% protein 5-6% <1% carbohydrate <<1% vitamins
essential nutrients
- carbohydrates
- vitamins
- fats and oils
- minerals
- proteins
- water
essential nutrients either
- cannot be made by the body
- can’t be made at a rate sufficient to meet needs
- are required in the diet
3 basic functions of nutrients
- energy (metabolize macronutrients into energy: protein, carbs, fat)
- structure (e.g. bones: protein, calcium)
- regulation (e.g. maintain body fluid balance with protein)
to express nutrients requirements
- RDA: recommended dietary allowances set by scientific evidence
- average daily level of intake sufficient to meet nutrient requirements of nearly all (97-98%) healthy people.
- RDA is one of the Dietary Reference Intakes
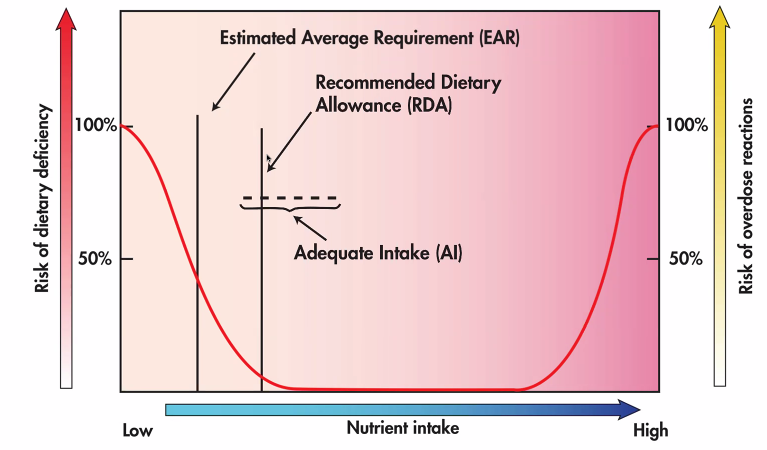
- without enough data, an AI range may be suggested
- RDA may shift over the years
scurvy: vit C deficiency
- causes hemorrhage under skin, lack of collagen causes teeth to fall out
digestion
- physical digestion: moving and grinding of food (mouth, stomach)
- stomach is the primary site of physical digestion
- chemical digestion: use of enzymes to break down food (stomach, pancreas, gallbladder, small intestines, large intestines)
- except carbohydrate, which begins in the mouth (enzymes)
- small intestines is the main site of chemical digestion
- small intestines are also a site of absorption made of villi
- villi maximizes surface area
- microvilli (parts of villi) draws nutrients into the bloodstream
60% of body weight is water 2/3 is intracellular 1/3 is extracellular
electrolyte distribution controlled via kidneys → fluid balance regulated
Week 1 module (proteins)
-
Magendie’s experiment: Nitrogen is essential in diet.
-
All types of proteins contain nitrogen, and they are the only type of macronutrient containing nitrogen.
-
Proteins fold differently depending on their amino acid sequence. Amino acids are connected by peptide bonds. Different fold patterns fulfill different functions in the body.
-
Amino acid = amino group + carboxyl + R group (20 possible R groups, meaning 20 possible amino acids)
-
How the R groups interact with each other determine how the protein folds.
-
Essential Amino Acids (EAA): 9 amino acids that cannot be made in the body
-
other 11 are not essential but can still serve as nitrogen sources.
-
Protein functions
- Structure: collagen = 1/3 of body proteins, etc
- body can make its own collagen as long as protein intake is enough; no need for collagen supplements
- energy
- 4 kcal / g proteins
- 15% of energy
- body cannot store proteins directly
- regulation
- make hormones - insulin
- make enzymes - catalyze reactions in the body
- immune system
- body fluid balance - fluid balance proteins move water into and out of cells; protein deficiency can cause edema—trapped fluid in body tissues
- Structure: collagen = 1/3 of body proteins, etc
-
protein digestion
- stomach acid denatures / unfolds proteins; cooking also denatures
- pancrea releases enzymes to break peptide bonds, we now have amino acids
- small intestine walls absorb most amino acids (EAA + NEAA); we also digest some old intestinal tract protein
- destination = liver / muscle / body cells
- protein turnover: proteins are constantly being built and broken down in cells (recycled so that we always have some leeway for new needs, e.g. injuries); this process is not completely efficient, so we need a constant supply of proteins for our diet.
- turn over rate
- fast rate (every few days) — intestines, immune system (WBC) (significantly impacted by protein deficiency since they need to be constantly rebuilt)
- medium rate (every several weeks/months) — muscle, skin, RBC, etc
- slow rate (months) — brain, central nervous system (protected against protein deficiency since they don’t need to be replaced that often)
- Dead-end protein: some proteins cannot turnover (e.g. hair, nails, top skin layer, stool); they must be replaced in diet
- After making enough NEAA, the body excretes nitrogen through urine and make use of carboxyl groups (use as muscle fuel or converted to fat)
- turn over rate
- Extra protein intake (e.g. protein powder) does not increase protein synthesis.
Week 2 module (proteins + nutrition)
Protein Deficiency
- protein deficiency / consequences of a low protein diet
- plant-based diet (if not planned properly) can be low in one or more EAA
- check diet for its protein quality (amount of EAA), especially when the diet is for infant / child (rapid growth).
- growth stages
- early development (gestation to toddler): cell growth by numbers
- needs significant amount of proteins
- very vulnerable to deficiencies
- severe protein deficiency may cause irreversible damage: intellectual disability or stunting of growth
- later development
- brain almost done growing (95% by mass)
- cell growth by cell size
- some protection against deficiency due to more slow turnover proteins
- protein deficiency issues are reversible but can still do some damage due to the expected rate of growth
- potential issues: edema (bad fluid balance), intestinal proteins (not enough fast turnover proteins, which in turn cause issues with nutrient absorption), distended abdomen (accumulating fluids, and fatty liver—fat needs protein carrier to travel in blood); risk of infection (immune system uses fast turnover proteins)
- protein deficiency types
- Kwashiorkor: inadequate protein intake of first-borns after weaning breast milk; edema, infections, etc
- Protein-energy undernutrition (PEU): inadequate protein and energy intake; bad protein and protein synthesis; body breaks itself down (e.g. muscle) for fuel
- early development (gestation to toddler): cell growth by numbers
Protein Intake Recommendation
- Goal: get nitrogen and 9 EAA
- Calculate RDA
- Step 1: Calculate a minimum
- measure average healthy person’s (70 kg male/female) nitrogen loss
- urine
- skin dust
- nails
- etc.
- determine how much “perfect protein” (contains all 9 EAA) is needed to make up for protein loss
- perfect proteins: egg, breast milk
- measure average healthy person’s (70 kg male/female) nitrogen loss
- Step 2: Adjust for population variability
- add 2 standard deviations to protein needs
- Step 3: Adjust for diet quality
- Since different foods contain varying amounts of EAA, we need to increase the previous protein needs to account for that
- Divide by average weight
- RDA for protein is 0.8 g protein / kg body weight
- Step 1: Calculate a minimum
- Factors of protein needs
- growth
- relative protein requirement per unit body mass: infant (~2g/kg) > child > adult
- pregnancy
- additional 25g/day
- grow placenta, lactation, etc
- injury & illness
- exercise
- 50% above RDA
- growth
Protein DV (daily value)
- Protein DV: 50 g/day for 2000 kcal diet
- complete protein
- digestible
- contains 9 EAA
- EAA content is proportional to need
- examples
- eggs (perfect)
- beef (sat fat!)
- poultry
- dairy (sat fat!)
- fish
- soybean
- incomplete protein: proteins that are either low in one or more EAA or do not provide them in proportion to human needs
- examples
- seeds
- grains
- beans
- nuts
- examples
- protein quality test
- indirect
- Protein Efficiency Ration (PER)
- feed test protein to lab rats
- measure growth
- PER = weight gained / protein eaten
- higher PER means higher quality protein
- Protein Efficiency Ration (PER)
- direct
- Chemical Score
- directly measure EAA levels using special machine
- compare relative EAA richness to egg white
- chemical score of a food is its lowest relative EAA (LAA—limiting amino acid) content percentage
- Chemical Score
- indirect
- pair foods with different LAA
Plant-based eating patterns
- plant-based diets
- vegetarian/vegan: no animal-based products
- veggie: limited animal-based products
- Plant-based diets have lower disease risks and provides other health benefits
- Protein Combining: Vegetarian sources are mostly incomplete proteins, so we need to consume sources with different LAA
- e.g. 1.25 cups rice + 1 cup lentils ~= 3 oz chicken
- complementary proteins are those that have different LAAs
- plant-based meat (similar taste and sometimes nutritional value to meat, but not necessary better due to processing)
Energy Value of Foods
- measuring energy
- combustion
- consumption by living animal i.e. rat (measure heat emitted)
- kcal = Cal = kilocalorie = 1000 cal
- use bomb calorimeter to measure heat of combustion of a food, which correlates to its chemical/potential energy, but not necessarily its physiological fuel value
- Body consumption is not 100% efficient, so some energy is lost during digestion. The actual energy gained is the “physiological fuel value”.
- proteins lose more heat content during digestion (indigestible lost to stool, and excrete nitrogen in urine)
- common physiological fuel values
- carb: 4 kcal/g
- protein: 4 kcal/g
- fat: 9 kcal/g
- Food label calorie amount is physiological fuel value
- Fiber cannot be digested, provides 0 kcal/g
Energy Needs
- Basal Metabolic Rate (BMR): energy needed to maintain basic body functions (e.g. beating heart, essential organ function)
- Activity: energy needed above BMR
- Thermic effect of food (TEF): energy needed to digest food, very small
- Growth: energy needed for children/infant growth
- calorie balance: intake = output
- 1 lb of fat = 3500 kcal
- Calculate BMR
- to measure: person at rest, fasted 12 hours, 24 hours without exercise, room temperature
- use constants and do dimensional analysis to convert to kcal/day
- male: 1 kcal per kg body mass per hour
- female: 0.9 kcal per kg body mass per hour
- calorimeter room: collect gas sample (CO2 and O2) to measure calories burned
- BMR factors
- age: consistent during adulthood, but after 60 BMR decreases 0.7%/yr
- fasting: decreases 10-20%
- exercise: increases BMR (variable effect)
Energy Costs of Activity
- activity profiles vs energy needed for activity as percentage relative to BMR
- sedentary (30%)
- light (50%)
- moderate (70%)
- strenuous (100%)
Thermic Effect of Food
- Assume it’s about 5% of total caloric intake
- TEF approx 50-200 kcal
- To estimate, TEF = 5% of (BMR + activity)
Week 3 - Carbs
Simple Carbs/Sugar
- carbohydrate: “energy nutrients”
- important to ability to be active
- hydrated carbon, C, H, O
- plants converts sunlight energy to carbs, carbon ring hydrated with water
- carbs can support energy, structure, and regulation needs
- workout uses carbs and fat for fuel
- chemical structure
- a (mono)saccharide is a sugar unit consisting a 6-carbon ring, potential energy stored in bond, 4 kcal/g
- simple sugar: monosaccharide or disaccharide
- monosaccharides: 1 carbon ring
- called simple sugar
- glucose: basic sugar unit (found in blood, starch, half of structure of table sugar)
- fructose: fruit sugar, slight chemical difference compared to glucose, sweeter at cold temps, also sweeter than glucose
- galactose: half of structure of milk sugar (disaccharide)
- disaccharides: 2 rings
- sucrose: most common in food supply
- glucose and fructose combined
- maltose: found in beer, malt, milk shakes, seeds, bean sprouts etc
- glucose + glucose
- lactose: found in milk and all dairy products
- glucose plus galactose
- products
- honey contains a mix of glucose and fructose and sucrose, plus some antioxidants
- high fructose corn syrup: mix of glucose plus fructose (sucrose without the bond)
- too much free fructose from the syryp leads to inflammation
- fruits that naturally contains fructose also comes with a lot more nutrients (e.g. vitamins, fibers, minerals, etc); juice drinks may taste the same but offer little desired nutrients due to the excessive added sugars (which is linked to increased disease risks).
- sucrose: most common in food supply
Complex Carbs
- polysaccharides: multiple simple sugar units bonded together
- starch: formed from multiple glucose units
- vegetable, grains, seeds, beans, potatoes, bread, rice, pasta, cereal, etc
- also found in unripe fruit
- fiber: long chains of monosaccharides like glucose, with a different bond angle; humans cannot digest fiber for energy, but fiber facilitate digestion
- glycogen: body’s storage form for carbohydrate-based energy
- stored in muscles
- glucose bonded in chains, with many branches
- glycogen may deplete during exercise
- not found in food source
- stored with water, takes up lots of space, body can store only a limited amount
- food examples
- plain pasta: polysaccharide (starch)
- fruits: monosaccharide (fructose), polysaccharide (fiber from skin)
- bread: polysaccharide (starch, fiber)
- yogurt: disaccharide (lactose)
- energy drinks: depends on type of sweetener used, but most likely monosaccharide (glucose) or dissacharide (sucrose)
Carb Digestion
- mouth: salivary amalase breaks down starch into disaccharides (maltose)
- stomach:
- acidic environment stops the salivary amalase
- breaks food into liquid
- small intestine
- pancrea secretion (enzymes: maltase, sucrase, lactase) breaks disaccharides into monosaccharides
- monosaccharides get absorbed into small intestine wall
- fiber gets discarded through stool
- lactose intolerance: lack of lactase
- intestine bacteria digest undigested lactose and release gas, causes bloating, cramping, etc.
- 10% young adults are diagnose
Fiber Benefits
- fiber provides structure to plants
- the fact that it is indigestible gives a few health benefits
- two types of fiber
- water-insoluble fiber:
- cell wall material
- cellulose
- hemi-cellulose
- sources: whole grains, vegetables, beans
- holds water and bulks up the intestine and speeds up intestine, softer to pass, relieve constipation, reduces risk of colon cancer (pass carcinogen quicker), lower risk for herrhoids and diverticulitis
- lack of water-insoluble fiber ingestion may cause chronic constipation, which may cause hemorrhoids (enlarged veins in/around anus); it may also cause issues to intestinal linings like diverticula (trapped waste in intestine in the form of pouches; causes inflammation, cramping) & diverticulitis (may also leak pouch content into body cavity)
- water-soluble fiber
- sources: fruits, oats, beans
- gums, pectins
- stomach-filling by surrounding sugars and slows sugar absorption into bloodstream → lowers risk for blood disease and type 2 diabetes
- maintain better blood glucose
- has a role in weight maintenance (more easily full → less overeating)
- forms gel
- binds cholesterol and help control/reduce cholesterol level
- water-insoluble fiber:
- whole grain
- bran layer (outside), hull fiber
- starch contents
- germ: nutrient rich
- common sources: whole grains, fruits (dried), vegetables, beans (legumes)
- if fiber presence in diet is low, don’t suddenly increase intake
- 38g/day for males, 25g/day for femals; 28g used for daily value
Carb as Energy
- digested monosaccharides go to the livers and get converted all to glucose, then they get transferred to muscle cells either to be used for energy or get stored as glycogen
- insulin need for glucose entry into cell
- insulin released after meal
- under 100 mg/dL for healthy individual
- blood glucose level rapidly rise after meal
- type 1 diabetes - pancrea not making enough insuilin
- generally genetic or suffer from
- need insulin replacements (injections or pump monitor)
- type 2 diabetes - insulin resistance / cells not responding to insulin (~90% of cases)
- receptors not responding to insulin, but can be improved with exercise
- cells think they are starving and makes you eat more, leading to high blood glucose level
-
126 normal BGL, often >200 post-meal
- cardiovascular disease (damage to artery walls and blood vessels in general)
- poor circulation (amputation)
- loss of eyesight
- infection (sugar rich blood fueling bacteria growth)
Regulating Carb Intake
- use as energy
- (anaerobic metabolism) break C6 (glucose) in half (C3)
- used by brain and nerves, and muscles during high intensity exercise
- (aerobic metabolism) break C3 to form CO2 and C2 for energy
- use C2 in citric acid or TCA cycle to break bonds to get energy
- 4kcal/g + H2O + CO2
- (anaerobic metabolism) break C6 (glucose) in half (C3)
- excess carbohydrates get stored in the liver as fat (carb: unused C2 units stored as fatty acid) after replenishing glycogen stores
- carbohydrate depletion
- glycogen only lasts a day at rest
- occurs with
- fasting
- no carbs in diet
- no insulin (diabetes)
- body’s solution: make glucose (expensive)
- convert body proteins into amino acids
- strip off nitrogen in amino acids (increased N in urine)
- use the left-over structure get some carbon units from fatty acid to make glucose
- very expensive, since we are breaking down proteins (lose body mass) and spend some more energy to make glucose
- low carb diet
- carb <50g/day
- accompanied with low intake fiber, vitamins, minerals
- constpiation, bad breath (50% of low-carb eaters)
- loss of weight with shift in energy use (glycogen depletion → water loss)
- loss of muscle mass
- more carbohydrates needed for increased activity (e.g. exercise)
- natural sugar: intrinsic sugar
- lactose in dairy
- fructose in fruit
- added sugar
- table sugar
- corn syrup
- brown sugar
- molasses
- …
- linked to
- high blood sugar
- cognitive impairments
- …
- recommends: <10% of total calorie intake
- brain prefers glucose as source
- gluten-free diet
- gluten
- protein found in wheat, rye barley
- grains contain gluten
- Celiac disease
- gluten intake causes intestinal tract inflammation and damage
- symptoms: diarrhea, vomit, abdominal pain, skin lesions, dermatitis, depression, fatigue, joint pain
- gluten
Fat
Intro
- fat
- often villified
- expected 30-35% total calories in diet
- excess fat linked to chronic disease (heart) & cancer (breast, colon)
- fulfills all three roles of nutrient: energy, regulation, structure
- energy source (270,000 kcal per year, or 30000 g fat)
- regulation (hormones, sex hormones)
- structure (thermal insulation)
- fat cell is filled with fat
- triglyceride (TG)
- three linearly bonded carbon (glycerol backbone)
- each C binds to a fatty acid (don’t have to be the same)
- basic unit of fat in food and body
- all fatty acids are chains of carbon (often even number of C’s)
- short, medium, long chain fatty acids
- the majority fatty acid determines the phase of fat at room temperature
- saturated fatty acid
- chain of carbon (complete with hydrogens) with an acid gruop at end (2 O and 1 H)
- usually even C’s (6, 12, up to 26)
- common saturated fatty acid: palmitic (16C), stearic (18C; found in animal)
- solid at room temp
- more stable than unsaturated fat (coconut needs this to grow in tropical climate, otherwise the oil would go bad)
- unsaturated fatty acid
- missing hydrogens in carbon chain, some carbons are missing hydrogens (uses double bond to make up for the loss)
- due to the double bond’s angle, unsaturated fat is bent
- in an 18:1 fatty acid, 18 represents number of carbons and 1 represent the number of C=C double bonds
- monounsaturated: 1 double bond
- Oleic acid (18:1) / Omega-9 (9th carbon is the double bond)
- not dietarily essential (body can make)
- good for heart health
- olive oil, canola oil, avocado
- Oleic acid (18:1) / Omega-9 (9th carbon is the double bond)
- polyunsaturated: multiple double bonds
- essential (body can’t make)
- linoleic acid (18:2) / Omega-6 (first double bond is on 6th carbon in chain)
- found in vegetable oils (corn, sunflower, soybean, safflower, sesame, nut oils)
- recommended 12-17g/day
- linolenic acid (18:3) / Omega-3 (3rd carbon has double bond)
- found in flaxseed oil and meal (whole flaxseeds are not digestible), fish, seafood; small amount in nuts, canola, soybean oils
- limited source
- anti-inflammatory effects
- recommended 1.1-1.6g/day
- types
- EPA
- DHA
- ALA (less important, common in plant food sources)
- too little Omega-3 has bad health effects
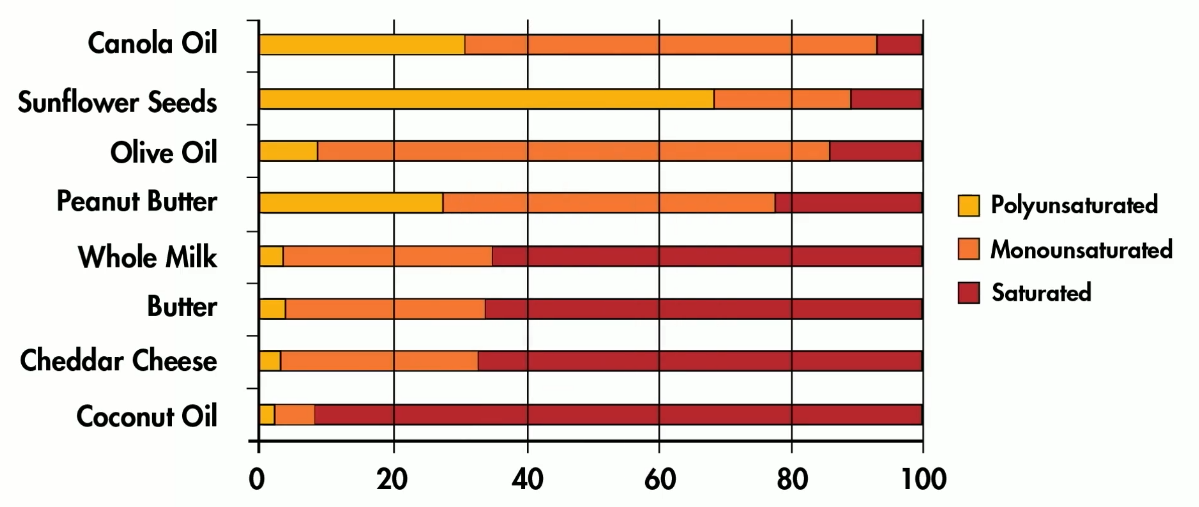
- a food is saturated if it has a majority (2 out of 3) of saturated fatty acid, likewise for unsaturated
- oils with polyunsaturated fats
- corn oil (18:1 and majority 18:2)
- flaxseed oil (18:2 and majority 18:3)
- fish oil (majority 18:3, 22:4)
- fish need unsaturated fat (more liquid at cold temperatures)
- need for unsaturated fatty acids
- membrane structure
- brain development & integrity
- Omega-3 is neuroprotective (e.g. against Alzheimer’s)
- needed to make prostaglandins: hormone-like substances needed for inflammatory response (e.g. clean up injury) and blood clot formation
- some prostaglandins promote inflammation
- Omega-6 is more pro-inflammatory, Omega-3 is more anti-inflammatory; balance is important
- essential fatty acid deficiency
- causes
- person is fed through a tube with insufficient nutrients
- restrictive diet with minimal fat intake
- limited bowel function
- causes
Fat in food
- majority of fatty acid type determines the whether the food fat is saturated/unsaturated
- animal
- saturated fat
- low 18:3 (linoleic, 18:3 (linolenic)
- exception: fish (18:3), chicken (half unsaturated fat), egg
- vegetable
- unsaturated fat
- high 18:1 (oleic), 18:2 (linoleic), very small amount of 18:3
- exceptions with high saturated fat content: coconut (>90% saturated), palm oil
- nuts primarily contain 18:2 (traces amount of 18:3)
Fats and food processing
- margarine
- hydrogenated fat (add hydrogen to vegetable oil to make it solid)
- converts unsaturated to saturated fat
- increased stability
- pretty bad for health
- some sat. fat doesn’t become saturated fully and becomes “trans” fats (as opposed to the cis configuration) and straightened out; double bond still exists
- trans fat intake associated with heart disease
- trans fat has no DV
- trans fat can be listed as 0g in food label if content is less than 0.5g/serving
- can be stored for longer
- unsaturated fats are unstable (weak to oxidation)
- oxygen can disrupt double bonds and make free radicals
- active free radicals destroy essential fats and taste
- hydrogenation adds hydrogen to saturate the unsaturated carbons and get rid of unstable double bonds
- unsaturated fats are unstable (weak to oxidation)
- hydrogenated fat (add hydrogen to vegetable oil to make it solid)
Fat Digestion
- insoluble in water
- no chemical digestion until intestine
- small intestine
- fat emulsificaiton: making fat soluble in water
- gallbladder secretes bile, which is made from cholesterol
- bile enables emulsification and enables digestion
- pancrea secretes pancreatic lipase which breaks down triglyceride
- fat drops form micelles
- fat droplet joins protein coat at small intestinal wall to form a chylomicron (type of lipoprotein = fat + protein) and enters circulation
- chylomicron transports fat to muscle and fat cell
- frequency changes with activity
- VLDL (very low density lipoprotein) gets sent from liver to different cells and deliver more triglycerides either produced by body or left over
Using fat for energy
- TG (triglyceride) → fatty acid (digested)
- put fatty acid through some path ways for aerobic metabolism → 9kcal/g + CO2 + H2O
- same output as carbohydrate output (aerobic)
Energy Storage
Following a meal
| Nutrient from food | Basic unit in body | Stored as |
|---|---|---|
| Carbohydrate | Glucose | Glycogen in liver / muscle |
| excess as body fat | ||
| Fat | tryglyceride / fatty acid | body fat store |
| protein | amino acid | protein replacement needs |
| excess as body fat |
Several hours after eating (energy consumption process)
| Energy source | Basic unit in body | Used for |
|---|---|---|
| glycogen | glucose | brain |
| energy for other tissues | ||
| fat stores | fatty acids | energy for other tissues |
Extended fasting (24hrs+); glycogen source depleted
| Energy source | Basic unit in body | Used for |
|---|---|---|
| body protein | amino acids | glucose for brain |
| discard N in urine | ||
| body energy | ||
| fat stores | fatty acid | body energy |
Using fat stores also produce ketones, which can also be used for body energy needs, but may be undesirable because build ups cause acidic environments (ketoacidosis)
Cholesterol
- important role, but we can make it in liver, so not dietarily essential
- use
- found in every cell membrane
- precursor to bile acids
- precursor to sex hormones (growth and reproduction)
- precursor to vitamin D
- all animal with liver will contain cholesterol
- self production: 1000-1500mg/day
- food sources: meat, organ meats, eggs, dairy, seefood, butter
cholesterol movement
- not soluble in water
- after fat gets delivered by VLDL, but since density shifted, VLDL becomes LDL and goes to body cells to deliver cholesterol to all body cells
- HDL from liver also picks up extra cholesterol the body doesn’t need (or take excess from LDL) to the liver
- cholesterol used to make bile, bile is used in digestion, and the cycle repeats
cholesterol transport condition (genetic condition)
- hypocholesterolemia leads to shortened lifespan since cholesterol deposits in body cells
Week 4 - minerals
Intro to Minerals
- mineral types: major vs trace minerals
- minerals are substances other than C, H, O, N (inorganic, since no carbon)
- comprises about 5-6% body
- stays in elemental form in body (Ca remains as Ca)
- dietarily essential
- nutrient function: structure, regulation
- minerals come from water/soil/rocks → { plants → animals (herbivores) } → humans (we eat both plants and animals)
- geographic location determines mineral quantity in food
- major/macro minerals > 0.01% body weight
- Ca, P, Mg, Na, K
- has a bioavailability issue
- trace/micro minerals < 0.01% body weight
- Fe, I, F, Se, Zn
- all in body fits in 1 tbsp
- generally required in small amounts <50mg/day
- function: mostly regulation, sometimes structure (fluoride)
- has a bioavailability issue
- bioavailability: amount of a nutrient that can be absorbed by the body
- mineral bioavailability range: <2% to >60%
- macronutrient availability range: 90-95%
- factors
- growth: increase
- pregnancy: same or increase for different minerals
- aging: same or decrease for different minerals
- medication: depends on medication and mineral
- fiber (>50g): same or decrease for different minerals (e.g. decrease for iron)
- mineral form: depends
- food factors and combinations: depends (e.g. vitamin C can increase iron bioavailability)
Calcium
- most abundant in body, 40% body mineral mass, 2% body weight
- function
- bone and teeth structure (99% of body Ca) Ca & P form mineral salt hydroxypatite in bone, collagen absorbs shocks, etc
- blood clot process
- muscle contraction (esp. heart) and nerve function
- deficiency
- no calcium in diet
- body wants to maintain regulatory role (body draws out calcium cache)
- Ca homeostasis
- hormones / vitamin D talks to intestine (Ca absorption / bioavailability), bone (calcium bank), kidney (calcium excretion)
- bone development and maintaenance
- cortical bone: form the shaft of bones and outer mineral coating
- trabecular bone: honeycomb-like structure to support outer coating
- marrow cavity: center of bone containing bone marrow, manufacturing site of RBC
- blood vessels: calcium in and out (osteoplasts break down Ca for body needs)
- calcium stores no longer get built after 30, so calcium intake early in life is important
- chronic low intake on calcium does affect bone structure: osteoporosis
- long-term low calcium intake (or vit D)
- estrogen loss (menopause, amenorrhea), which is important for bone building
- inactivity
- genetics
- increasing age
- …
- 4-week deficiency results in lower calcium stores in bone to maintain blood calcium levels
- person loses height due to osteoporosis
- calcium deficiency
- child
- decreased skeletal growth
- soft bones
- rickets (slightly curved bone)
- adult
- osteoporosis
- weak/fragile bones
- child
- calcium bioavailability
- requires vitamin D for synthesis of a carrier protein in intestines
- 30% bioavailability
- increased bioavailability in youth, pregnancy, lactation
- decreased bioavailability during menopause (women, old age)
- calcium requirements
- adults: around 1000mg
- old adults: 1200mg
- food sources
- milk (1 cup = 300mg)
- cheese (1.5-2oz = 300-400mg)
- yogurt (8 oz = 450)
- tofu (4 oz = 150mg)
- molasses
- broccoli
- salmon (and other seafoods)
- tortilla
- fish sauce
- phytates (grains), oxalate (greens) decreases bioavailability of calcium to a very limited degree
Sodium & Potassium
- function
- electrolytes: fluid homeostasis, nerve impulse transmission
- attract H2O
- Na & K levels are controlled by hormones and kidneys
- Na pulls water outside and K pulls water into cells
- electrolyte deficiency is caused by sudden loss by body fluids (extreme exercise or high temperature)
- causes
- heavy sweating (primarily sodium lost)
- vomiting
- diarrhea
- symtoms
- lowered blood pressure, nauseous, dizzy
- causes
- bioavailability not an issue
- although people are supposed to consume more potassium than sodium, in reality people eat a lot more sodium compared to potassium, which is linked to heart disease
- excess sodium gets discarded by the liver in urine
- processed food loses potassium and gains a lot of sodium
- foods
- avocado (K)
- …
Iron
- function
- used for oxygen transport (one hemoglobin has four iron, which binds to oxygen)
- used for oxygen storage (myoglobin)
- deficiency
- body tries hard to not lose iron
- liver recycles iron from old/dead blood cells
- stores iron (e.g. in liver); women have low iron stores due to menstration
- if low, body can increases iron absorption (bioavailability)
- decreases undesired excretion of iron (i.e. by increasing absorption)
- anemia (“sick blood”)
- causes
- poor diet
- blood loss
- …
- symptoms
- low iron stores
- low hemoglobin
- poor oxygen transport (fatigue, smooth tongue, spooned nails/koilonychia)
- causes
- risk groups
- infants
- children
- women (child bearing years)
- body tries hard to not lose iron
- bioavailability
- gender: women have lower iron stores and higher bioavailability by default compared to men
- iron in food
- heme iron (flesh, blood): 20-30% bioavailable
- non-heme iron (plants, dairy, and some from meat): 1-10% bioavailable
- meal composition/food factor
- increase
- vitamin C increases bioavailability (e.g. orange juice)
- meat increases bioavailability of non-heme iron, because of a special protein factor
- decrease
- oxalate (organic acid in leafy greens) decreases heme iron availability
- phytate (organic acid in whole grains in seed form) decreases heme iron availability
- very high fiber (>50g) decreases heme iron bioavailability
- tannins (in coffee, tea, wine) decreases non-heme iron bioavailability
- RDA assumes 10% bioavailability
- 8mg/day for men, 18mg/mg for women, 27mg for pregnant women (dietary supplement a must)
- food sources:
- heme iron: liver, meat (dark poultry better than light poultry), blood
- non-heme: leafy greens (esp. those low in oxalates), breakfast cereals (which are also often fortified), grains (iron added required by law), beans, meat, dried fruits
- toxicity
- hemochromatosis: iron overload
- excessive absorption of iron, iron deposits in tissue, can lead to liver failure and cancer
- iron is pro-oxidant, which causes damage
- blood-letting and filter out iron
- supplements: decrease zinc absorption (avoid doses of iron >45mg)
- iron poisoning: leading cause of death in toddlers accidentally eating supplements
- hemochromatosis: iron overload
Zinc
- ”male” mineral
- function
- cofactor in >100 enzymes reactions (i.e. works with enzymes to enable reactions and processes, like cell replications, especially growth and sexual maturation, would healing, immune function, taste perception, reproduction, etc)
- deficiency
- delayed sexual development
- impaired immune function (elderly)
- decreased taste perception (elderly)
- reduced sperm count (experimentally produced)
- delayed growth
- absorption/bioavailability
- whole grains in original grain form (e.g. in unleavened bread) contains phytate, decreasing absorption
- oxalate (greens) decreases bioavailability
- requirement
- 8mg/day (female), 11mg/day male
- source
- oysters
- fortified breakfast cereal
- beef
- turkey
- wheat germ
- garbanzo beans
- milk
- kidney beans
Iodine
- function
- incorporated into thyroid hormones, which direct use of oxygen → sets MBR, heat production, reproduction, growth, etc
- deficiency
- iodine deficiency documented since 3000 BC in China
- intake directly linked to geographical location
- path through food chain: water/soil → plants → animals → humans; if iodine presence in soil is low, then humans get iodine deficiency
- low thyroid hormone levels prompts pituitary gland to signal a thyroid gland size (“goiter”)
- symptoms
- enlarged neck
- sluggish feeling
- weight gain (lower oxygen use)
- pregnancy
- infant has cretinism
- viewed by some cultures as attractive
- some cultures view it as a sin (e.g. adultery)
- 1920s discovered I deficiency was cause of goiter
- US gov’t made Morton company to fortify table salt with iodine
- symptoms
- still prevalent issue world-wide
- requirement: 150 mcg/day
Fluoride
- function: structural + regulatory
- F incorporated into bone and teeth mineral structure
- teeth become more resistant to decay (dental caries)
- dental caries (tooth decay / periodontal disease)
- regulatory because tooth issue can also lead to heart disease, etc
- deficiency
- fluoride is present water supply (either natural or added through fluoridation)
- requirement: 4 mg/day
- source: water, toothpaste, mouthwash, communities with fluoridated water supply
- toxicity: excess F (in water supply, e.g. North/South Dakota) causes fluorosis—mottling of teeth (from chalky appearance to dark stains)
Week 6 - Vitamins
Vitamin Intro
- Vitamin: micronutrient that is organic (has C)
- function: regulation
- 13 different vitamins (each with unique structure)
- vitamin needs differ among species (some need vit C, some don’t, some can even produce some vitamins by themselves)
- water-soluble (e.g. vit C) vs fat-soluble (e.g. vit A)
- water-soluble vitamins
- B vitamins
- C (ascorbic acid)
- found in watery part of cells
- fast turnover in body (approx 24-48 hours, therefore regularly needed)
- excess is filtered from blood and discarded through urine
- function as enzyme helpers (coenzymes); facilitate enzyme action
- deficiency timeline
- vitamin deficient diet
- tissue depletion (3-4 weeks)
- biochemical lesions (4-6 weeks)
- clinical signs (6-8 weeks)
- skin changes
- intestinal changes
- tongue (smooth, purple)
- fatigue
- B vitamins
- B1: thiamin
- B2: riboflavin
- B3: niacin
- B5: pantothenic acid
- B6: pyridoxine
- B7: biotin
- folate / folic acid
- B12: cyano-cobalamin
- fat-soluble vitamins
- A, D, E, K
- stored/found in fatty parts of cell and body (e.g. within cell membrane)
- slow turnover—less frequently needed (deficiency can take 5 years to show up) than water-soluble vitamin
- excess is stored, but high amounts can be toxic
- function in more general roles (not coenzymes) across different body systems
- absorbing from food
- high heat often damages vitamins (e.g. vit. D1), but they are taken into account into the RDA
- vitamins are often instable in food (e.g. some can be damaged with exposure to oxygen)
Thiamin (Vitamin B1)
- water-soluble
- coenzyme in carbohydrate and energy metabolism
- increased carbs consumption means more thiamin needed (e.g. active people, athletes)
- deficiency: found among cultures relying on grains for majority of calories (rice, corn, wheat, etc)
- white rice loses the hull from brown rice (which contains thiamin)
- deficiency disease: Beriberi
- not enough energy (can’t use energy from carbs)
- CNS dysfunction
- muscle fatigue
- heart failure
- RDA: 1.1-1.4 mg
- food sources
- grains
- meat, poultry, fish
- liver
- pork (high)
- legumes, beans
- breakfast cereals (mostly enriched)
- high heat destroys thiamin
Niacin (Vitamin B3)
- water-soluble
- coenzyme in fat, carbohydrate, and protein energy metabolism & fat production
- if high-quality proteins, consumed, body can make its own niacin
- body can convert tryptophan (amino acid) to niacin
- deficiency disease: Pellagra
- history
- In 1900s in the South, diet was mainly: grits (corn), black eyed peas, salt pork (mainly pork fat)
- low-niacin diet
- low bioavailability in corn
- poor-quality protein (black-eyed peas, salt pork)
- poor protein prevents conversion of tryptophan to niacin
- estimated killed 150k people in first half of 20th century
- In 1900s in the South, diet was mainly: grits (corn), black eyed peas, salt pork (mainly pork fat)
- dermatitis
- diarrhea
- delirium/dementia
- death if not treated
- history
- food sources
- meat
- fish
- poultry
- refined (enriched)/whole grains
- cereals (enriched)
- nuts
- beans
Vitamin B12 & Folate (Folic Acid)
- water-soluble
- work together
- function
- coenzymes in growth and turnover of new cells
- especially affects high turnover cells (blood, immune, intestine)
- Genetic material replication
- needed for metabolism of protein metabolite homocysteine (if not metabolized/removed, high levels of it damages blood vessels and increases heart disease risk)
- vitamin B12 specific: needed to produce/maintain myelin sheath
- coenzymes in growth and turnover of new cells
- food sources
- Vitamin B12 special considerations
- need a special factor made in stomach for absorption (Intrinsic Factor/IF made by parietal cells)
- mineral cobalt is part of B12 structure
- water-soluble, but can be stored liver (approx 2 year supply)
- found only in animal-based food or fermented food (e.g. kimchi, yogurt)
- deficiency
- high turnover cells can become damaged, e.g. blood
- ”pernicious amenia” (different than iron deficiency anemia)
- folate or vitamin B12 deficiency causes nerve damage and can cause paralysis
- foor folate intake pre- and during early pregnancy may lead to birth defects (neural tube defects)
- all grains now enriched with folate
- RDA:
- 19+ y/o:
- B12: 2.4 mcg/d
- folate: 400 mcg/d
- pregnancy:
- B12: 2.6 mcg/d
- folate: 600 mcg/d
- lactation:
- B12: 2.8 mcg/d
- folate: 500 mcg/d
- people of old age produces less stomach acid, so might need more vitamin B12
- 19+ y/o:
- Pregnancy and change in nutrient needs
- protein
- iron
- folate
- vitamin B12
- calcium do not change with pregnancy (bioavailability/absorption increases during pregnancy)
- folate food sources
- liver
- green veggies, leafy greens
- orange/citrus juices
- beans/legumes
- enriched/fortified grains, breakfast cereals
- vitamin B12
- meat
- milk
- fish
- fermented foods (kimchi, pickles, etc)
Whole grains, refined grains, and enrichments
- enrichment program started in 1940s
- added to refined grains
- niacin
- iron
- thiamin
- riboflavin
- folate (1996)
- whole grain kernel constituents
- hull: water-insoluble fiber, B vitamins (e.g. thiamin, niacin), minerals, iron
- starch: carb
- germ: minerals, B vitamins, vitamin E
- milling/refining removes hull and germ from grain; loses much of fiber, B vitamins (1,2,3,6,folate), iron, zinc, magnesium
- enrichment program requires adding B vitamins (1,2,3, folate), iron to levels in whole grain, though refined grains are still missing B6, E and certain minerals, fiber, lignan, plant stanol & sterols (helps heart disease), resistant starch, antioxidants, phytate (not great, but still has some health benefits), inulin and fructoligosaccharides
- Eating whole grains are better than eating constituent nutrients from supplements.
- whole-grain examples: brown rice, whole wheat, popcorn, barley, oats, whole corn, millet
Vitamin C (ascorbic acid)
- water-soluble
- function: regulatory
- needed in the formation of collagen protein (structural protein), which is needed for bones, blood vessels, gums
- aids in iron absorption
- antioxidant: protects fat and other substances against oxidation
- vitamin C, E, beta-carotene, vitamin A, etc
- prevents oxidation of in organelles e.g. ER, cytoplasm (water-soluble, e.g. vitamin C)
- oxidation can be responsible for chronic diseases
- deficiency disease: scurvy (fatal)
- history: deficiency of vitamin C influenced history (new world exploration; 1/2 of sailors and slaves on ships dead due to scurvy); sailors, spice traders, pirates suffered from scurvy
- develops after 7-8 weeks of deficiency
- swollen, bleeding gums (really easy to bleed)
- loose teeth
- sore, painful joints (tendons and ligament cells are not being replaced properly)
- fragile bones
- hemorrhage under skin
- death if not treated
- requirements
- most animals can make it from glucose, but humans and primates require vitamin C
- RDA: women (75mg/d), pregnant (85 mg/d), men (90 mg/d), smokers (additional 35 mg/d)
- tolerable upper limits: 2,000 mg/d
- food sources
- all kinds of fruits (kiwi, orange, strawberry, cantaloupe, etc)
- orange juice
- tomatos, grapefuits
- broccoli, cauliflower, pepper
- supplement tips
- higher intake of vitamin C (200-500 mg/d, but only from food) may reduce risk for CVD, cancer, and other age related disease
- vitamin C may or may not reduce common cold symptoms/risks (no clear evidence)
Retinol (Vitamin A)
- fat-soluble
- function
- vision cycle: ability to perceive black/gray/white colors and night vision; sudden change of brightness
- 1% of body vitamin is in the back of the eyes
- maintenance of epithelial tissue - “covering tissue”; examples:
- skin
- sinus/lung lining
- urinary tract
- intestine
- etc.
- vision cycle: ability to perceive black/gray/white colors and night vision; sudden change of brightness
- food beta-carotene can reduce risks of age-related diseases
- deficiency
- night blindness: can’t see at night
- xerophthalmia: irreversible eye condition
- cornea sloughs off, causes blindness
- 500k children < 5 years old go blind yearly
- infection of epithelial tissues
- skin begins to exude keratins; hyperkeratosis
- lungs become more prone to infection
- etc
- stunting of growth in children
- food sources
- animal products & milk, etc
- plant source: carotene (especially beta-carotine) can be converted/split into vitamin A
- beta-carotine enriched rice / golden rice (GMO)
- all kinds of fruits and vegetables
- requirement
- female: 700 RAE, male: 900 RAE
- food sources
- liver (3oz - 9000RAE); beware of poisoning though
- egg (84RAE)
- milk (100RAE)
- orange, yellow fruit (100+ RAE): cantalope, apricot, papaya, etc
- orange, yellow vegetables (1000+ RAE): carrot, butternut squash, pumpkin, etc
- unit: RAE (retinol activity equivalent)
- animal vitamin A: 1 mcg animal vitamin A
- supplement: 2 mcg (beta-carotene)
- food: 12 mcg
- hypercarotenosis: beta-carotene itself is not toxic, but will color the skin yellow; excess beta-carotene can be excreted (not vitamin A yet)
- vitamin A toxicity
- stored in liver and fatty tissue
- causes birth defects (neural tube)
- enlarged liver
- headache
- peeling of skin
- gingival discoloration
Vitamin D
- fat-soluble
- function:
- calcium metabolism
- calcium absorption (builds protein to take up calcium in intestines)
- regulation of blood calcium levels (kidneys)
- bone mineralization by maintaining calcium concentrations
- emerging roles
- cancer prevention (low circulating of vitamin D linked to increased cancer risk)
- protection against CVD and hpertension
- preventino of autoimmune diseases
- calcium metabolism
- deficiency
- problem found in areas with reduced exposure to sunlight
- normally: sunlight + liver + kidney + cholesterol → make vitamin D → can absorb calcium → no rickets
- rickets: lack of mineralization of bone (soft bones, overgrowth of cartilage, enlarged head)
- osteomalacia: softening of the bones
- requirements
- darker the skin, the more sunlight needed (light skin: 30min/d; dark skin: 2hr/d)
- sunblock prevents vitamin D formation (oct - mar, insufficient UVB ray in locations with latitudes north of Los Angeles)
- increases with age (1-70y/o: 600 IU; 70+ y/o 800IU)
- old age: less outdoors activity, liver/kidney funciton decreases with aging
- food sources
- fatty fish (300-500 IU/serving)
- fortified milk (400 IU/qt)
- mushrooms if exposed to UV (200 IU)
- eggs
- liver
- Toxicity: 2-3 times RDA is toxic to children—bone malformations and calcification of soft tissue
Vitamin E
- fat-soluble
- function:
- antioxidant that protects cell membranes from oxidation (especially those that are constantly exposed to high amounts of oxygen)
- lungs
- blood cells
- other cells: muscles (high exposure)
- Vitamin E sits in cell membrane and protects unsaturated fatty acid in cell membrane from lipid peroxidation (unsaturated fat is not stable in presence of oxygen)
- antioxidant that protects cell membranes from oxidation (especially those that are constantly exposed to high amounts of oxygen)
- deficiency: hemolytic anemia—red cells break
- rare
- takes 7 years to become deficient
- low intake may lead to weakened cells (prone to carcinogens, disruption in brain/alzheimer’s, etc)
- aging leads to poor intake of vitamin E
- requirements
- 15 mg (22 IU)
- tolerable upper limit (1000 mg/d)
- less dangerous toxicity effects (flu like symptoms; bleeding/bad clotting ability)
- food sources
- vegetable oils
- nuts
- seeds
- whole grains (germ)
- note that enrichment program does not add vitamin E, so enriched refined grains are not a food source.
- avocado
Dietary Supplements & Safety
- foods are usually better than supplements (higher bioavailability, etc)
- consider supplements if
- if calorie intake is <1,500 kcal/d (esp. female, elderly)
- if alcohol is heavily consumed
- if pregnant (very high iron need)
- if irregular eating habits & poor selection of food
- choose supplements that are around 100% RDA, avoid “mega-doses” (risks of toxicity)
- FDA’s definition of dietary supplement: contain at least one of the following: vitamin, mineral, herb or other botanical, amino acid, metabolite, plant/fruits concentrates, plant extracts, or dietary substance
- supplements are not very well regulated
- FDA: manufacturers may claim on labels:
- statements of nutrition support
- may claim effects such as “promotes structure” or “promotes function” but may not claim a “drug-like effect” or “disease cure”
- OK: promotes excretion regularity, helps promote urinary tract health
- not OK: laxative, protects against urinary tract symptoms
- FDA: manufacturer must have substantiation for claims, but not required to provide unless investigated
- supplements are not checked for quality and quantity of active ingredients (may have dangerous amounts)
- some supplements may negatively interact with prescription and OTC medication
- supplements may increase complication during surgery
- many supplements have unsafe side effects (not within FDA’s control); e.g. there is a few deaths associated with “5-hour energy” drink but it’s still on market
- supplement & legal information sites: FDA, FTC, NIH, sites without ads/affiliation, journals, Office of Dietary Supplements, etc
Week 7 - Cardiovascular health & nutrition
How heart diseases develops
- can develop at a young age
- general progression
- healthy artery
- lumen (opening)
- lining around lumen (endothelium)
- muscle around lining
- early injury
- LDL builds up on artery wall and builds up plaque
- atheroscelerosis
- narrowed lumen or opening
- fat deposits (cholesterol)
- plaque build up blocks up most of lumen
- healthy artery
- lipoproteins
- VLDL
- contains: triglyceride, cholesterol
- function: delivers triglyceride to cells
- LDL
- contains: triglyceride & cholesterol (rich)
- function: delivers cholesterol to cells
- HDL
- contains: triglyceride & cholesterol
- function: picks up extra cholesterol from cells or LDL, and return it to liver
- VLDL
CVD risk factors
- LDL oxidization can be caused by poor diet, smoking, inactivity, etc, which eventually spills and infiltrates artery walls and develops plaque
- platelets gather and clump up at the LDL oxidation / spill site, which could lead to heart attack
- coronary artery disease (atheroscelerosis): too much LDL oxidation causing major blockage in artery
- risk factors
- cigarette/smoking (unclear effects from drug smoking)
- vaping increases oxidation stress, so not necessarily healthier than cigarettes
- hypertension: more narrow & rigid artery walls, which reduces leeway of LDL oxidation
- hypercholesterolemia (high LDL, low HDL)
- dietary factor
- diabetes
- heredity
- age
- excess body fat (ab fat)
- male sex (males have increased risk; estrogen helps lower CVD risk)
- inactivity
- cigarette/smoking (unclear effects from drug smoking)
- how diet can help reduce CVD risks
- high water-soluble fiber consumption can help lower CVD risk by binding to and excreting cholesterol
- lower blood pressure
- reduce cholesterol in blood
- lower body fat
- mitigates type II diabetes
- mitigates metabolic syndrome
- metabolic syndrome: 3 out of 5 factors below:
- abdominal obesity (>35” for female, >40” for males)
- insulin resistance (above normal fasting blood glucose >100mg/dl)
- high blood pressure/hypertension (>130/80mmHg)
- high blood triglyceride
- low HDL levels
- risk of death increases non-linearly with cholesterol levels in blood (measured by summing LDL & HDL levels in blood)
-
200, steeper slope
-
300, risk skyrockets
-
- blood cholesterol levels
- desired: <200mg/dl
- borderline-high: 200-239 mg/dl
- high: >240 mg/dl
- ratio of LDL to HDL matters
- LDL
- desired: <100 mg/dl
- above optimal: 100-129 mg/dl
- borderline-high risk: 130-159 mg/dl
- high risk: 160-180 mg/dl
- HDL
- low: <40 mg/dl
- LDL
- Genetics influence cholesterol levels. Routine blood lipid panels recommended to monitor cholesterol in blood, since we can’t feel cholesterol’s effects until it’s too lates
Diet
- diet risk factor
- total dietary fat intake
- saturated fat intake increases risks (increases LDL)
- it’s not known whether saturated fat directly causes heart diseases
- unsaturated fat reduces risks
- cholesterol intake does not significantly influence blood cholesterol, so there’s no dietary cholesterol recommendation for healthy individuals
- protein intake; amino acids found in plants may be helpful
- water-soluble fiber
- other minor components
- fish oil (unsat. fat?)
- garlic (in large amounts) can reduce risks
- unfiltered coffee may oxidize LDL (reduced consumption causes LDL level to return to normal within weeks)
- wine (color compounds inhibit platelet action and prevents artery wall blockage)
- fat consumption
- recommended intake
- try to keep fat between 25-35% of total calories
- try to keep saturated fat to below 10% of total calories
- try to make monounsaturated fat 10%+ of total calories
- try to keep polyunsaturated fat to below 10% of total calories
- lower fat intake is typically associated with lower CVD risks, but the ratio of sat/unsat fat consumed and food sources/quality may modify risks (higher sat → higher risks)
- saturated fat & trans fat
- raises total blood cholesterol levels
- raises LDL levels
- increases coronary heart disease risks
- trans fat can also lower HDL levels
- note: coconut oil contains saturated fats and is not directly linked to reduced risks, do not consider it as a “health food”
- note: industrial replacement for trans fats
- saturated fat oil + polyunsaturated fat oil
- interesterified (IE) fats: converts liquid fats to solid fats by artificially rearranging the shape of triglycerides; currently not much known on its health effects
- monounsaturated fats
- lowers total blood cholesterol levels
- lowers LDL cholesterol levels
- neutral to HDL cholesterol level
- polyunsaturated fats
- lowers total blood cholesterol levels
- lowers LDL cholesterol levels
- lowers HDL cholesterol levels
- Since it lowers both LDL and HDL, it is not as healthy as monounsaturated fat
- Omega-3 is known to reduce for CVD risks.
- recommended intake
- reduce risk for heart disease with diet
- see fat consumption (previous bullet) > recommended intake
- salt < 6g (2,300 mg sodium)
- minimize alcohol intake (1 drink/day for females, 2 drinks/day for males); alcohol increases inflammation
- achieve a healthy body composition (reduce body fat, which is metabolically active)
- refer to AHA’s Life’s Essential 8
Week 8 - Body Composition
Obesity
- ”Health At Every Size” & size diversity
- behavior
- food & beverages
- physical activities
- genetic → inflammation
- environmental → inflammation
- obesity rates rising in US
- 73.6% are overweight/obese (BMI > 25)
- of those, 42.4% are obese (BMI > 30)
- 21.2% 2-19 y/o are obese
- $147B annual cost of obesity
- declining physical fitness
- 73.6% are overweight/obese (BMI > 25)
- BMI (kg/m^2)
- ranges
- healthy: 18.5 - 24.9
- overweight: 25-29.9
- unhealthy: >=30
- issues
- doesn’t account for body fat, water, muscle, waist size, bone density
- doesn’t factor age sex, race/ethnicity
- was not developed to measure health, especially on an individual basis
- ranges
- obese 5 y/o are 4 times as likely to be obese by teen years
- obese teenagers have higher risks of diabetes
- double burden of malnutrition:
- existence of both overnutrition & undernutrition
- policy changes needed
- ”first year 15”
- life style changes
- schedule
- sleep patterns
- food availability
- uncontrolled portions
- decline in physical activity
- life style changes
- impact of COVID
- mindless eating
- increased intake
- decrease in appetite
- eating to cope
- relapse of eating disorder
- increased alcohol intake
- why are obesity rates increasing
- caloric intake
- total calories
- caloric composition
- appetite
- calories absorbed
- psychological factors
- calorie output
- BMR
- TEF
- activity
- energy burned by non-exercise activity
- other factors
- physical
- economic
- social
- caloric intake
- body fat distribution
- upper-body
- apple-shaped: excess abdominal fat
- waist
-
40 males
-
35 females
-
- lower-body
- pear-shaped: excess hip/femoral fat
- upper-body
- abdominal fat
- subcutaneous fat
- visceral fat: excess can have extra pressure against organs
- health risks: obesity leads to excess adipose tissue, which contributes to a state of inflammation
- alzheimer’s
- mental health
- sleep disturbances (sleep apnea, etc)
- pulmonary
- CVD
- cancer
- type 2 diabetes
- gallbladder
- reproductive disorder
- neuropathy disordres
- osteoarthritis
- adipose cell: fat cell
- nucleus + fat droplet
- metabolicalic active
- secretes hormones
- lipoprotein lipase (LPL) used to communicate with body to deliver TG to cell
- factors that increase LPL activity
- fat deposit site
- hormones (pregnancy)
- weight loss
- exercise
- fat cell development
- critical periods: increase in fat cell number
- newborn: 3rd trimester - 1 year
- teen: adolescen growth spurt: 12-14 y/o
- adulthood: only fat cell size increase
- critical periods: increase in fat cell number
- weight loss
- fat cells only decrease in size during weight loss; they do not go a way
- the more fat cells present, the more LPL activity
- once obese, it gets difficult to go back
- body fat determination
- skin-fold thickness: skin-fold caliper
- underwater-weighing (hydrostatic weighing): fat floats in water; the more fat, the less the person will weight in water
- bioelectrical impedance: high resistance = high body fat
- DXA (dual-energy X-ray)
- Note: different error exists in every method, so try to track using one method consistently
Influences on Food Intake
- factors that affect calorie balance
- physical
- economic
- social
- brain influences
- CNS (hunger & satiety detection)
- hypothalamus (receives signals)
- ghrelin
- leptin
- insulin
- PYY
- NPY
- fatty acids
- amino acids
- serotonin
- glucose
- epinephrine
- brain chemicals (NPY, serotonin)
- hypothalamus (receives signals)
- peripheral factors
- hormones (e.g. insulin)
- fat mass & cell size (full fat cells send leptin to signal fullness)
- stomach: PYY, ghrelin (empty stomach uses it to stimulate hunger)
- exercise
- conditions
- pregnancy
- excess body fat (high LPL activity)
- eating disorders
- cancer (decreased appetite)
- psychological conditions
- environment factors
- time of day (lunch time prompts to eat even not hungry)
- eating cues (e.g. buffet)
- temperature (hotter = colder foods more attractive, etc)
- sleep deprivation
- late-night craving for energy-dense foods
- ghrelin levels increase
- may overeat the next day
- circadian rhythm
- lower appetite in morning, increased appetite in evening
- evolutionary design: eat more in evening since long hours of sleep ahead
- CNS (hunger & satiety detection)
Theories behind excess body fat
- calorie imbalance
- inactivity
- genetic
- truncated leptin protein can’t bind to leptin receptor
- other genes
- ”set-point”: fat cells need certain amount of TG
- metabolism - “thrifty” (some people can conserve more energy from food)
- diet composition (fiber, proteins increase fullness, etc)
- meal patterns (e.g. timing, skipping meal)
Changing body composition
- weight inclusive approach
- goals
- health is not unidimensional
- non-stimatizing health care
- weight is not ultimate goal
- guidelines
- do no harm
- create practices and environments that are sustainable
- keep a process-focus rather than end-goals, day-to-day qualify of life
- incorporate evidence in designing interventions
- include all bodies and lived experiences, a norm of diversity
- increase access, opportunity, freedom, and social justice
- given that health is multidimensional, maintain a holistic focus
- trust that people (and bodies) move toward greater health given access and opportunity
- goals
- weight loss study: people who lost weight and kept it for 1y did
- 78% eat breakfast daily
- 75% weigh themselves once a week
- 62% view <10h of TV per week
- 90% excercise about 1h/d
- key components of evidence-based body composition adjustment
- change energy intake
- energy in < energy out while satisfying all nutrient needs except caloric intake (or in > out if doing weight gain)
- make sure the diet is enjoyable/tasty
- minimize hunger and fatigue (sign that diet does not fulfill basic body needs)
- for weight gain: focus on high-quality protein and healthy fats, eat more often (as opposed to large meals)
- behavior modification
- changing eating behavior
- change response to environmental cues or avoid cues entirely
- e.g. avoiding passing the donut shop
- cognitive restructuring
- record why you are eating what you eat in a food diary
- look for common patterns, e.g. is there a mood relationship?
- reinforcement of behaviors (reward good dietary habits with non-food rewards)
- exercise
- calories out > in for weight loss
- weight gain can also use excercise for lean tissue mass
- increased metabolism
- better weight maintenance
- improved sense of well-being
- decreases risks of chronic disease
- physical activity (help energy expenditure and build lean body mass)
- change energy intake
- intuitive eating
- reject diet mentality
- honor hunger
- make peace with food
- challenge the “food police”
- discover the satisfaction factor
- feel fullness
- cope with emotions with kindness
- respect your body
- excercise and feel the difference
- honor your health with gentle nutrition
- ineffective weight loss
- very calorie diets
- reliance on formulas or special products (low carb/high protein or low carb/high fat diet)
- extremes in macronutrient restriction (e.g. very low carb intake)
- appetite suppressant drugs (unsafe and ineffective)
- surgical procedures
- Avoid rapid weight loss
- BMR decreases after weight gain
- weight likely to rebound
Week 8.5 - Special Topics
Alcoholism
- alcohol = 2-carbon molecule
- not a nutrient
- alcohol requires no digestion
- can directly move through stomach lining
- drinking with food helps slow down alcohol absorption & effects
- some minor enzyme digestion
- males have more enzymes and have less alcohol in bloodstream
- alcohol stored in liver
- C2 → TCA cycle (7 kcal/g)
- C2 → fat (stored)
- liver prioritizes alcohol digestion over all other functions
- metabolizing ability
- males have larger liver than females & more body water (dilutes alcohol), so they can process more of it
- human body can process 15g alcohol/h (i.e. 1 drink = 12oz beer) (but body size can affect this)
- genetics
- adaptation occurs with increased consumption
- liver problems when processing alcohol
- decreased ability to convert amino acids to glucose
- decreased protein synthesis (e.g. lipoprotein protein coat) → fat stays in liver becuase no lipoprotein can take them
- fat buildup if alcoholism
- how alcohol interferes body function
- ingestion: reduced appetite, substitution
- missing nutrients, increase risk of deficiency
- absorption: reduced or impaired absorption of micronutrients
- thiamin, folic acid, B12, iron
- metabolism: altered or impaired metabolism of micronutrients
- B3 (niacin), D, B6, A (special carrier protein needed from liver)
- excretion: alcohol increases urine production
- folate (folic acid), Zn, Mg, Ca, K
- ingestion: reduced appetite, substitution
- fetal alcohol syndrom (FAS): alcohol exposure during pregnancy
- irreversible facial feature changes
- smaller head, epicanthal folds, flat midface, smooth philtrum, low nasal bridge, small eye opening, short nose, thin upper lip, underdeveloped jaw
- irreversible facial feature changes
- alcohol is a type of empty calorie food: only an energy source, no essential nutrient contribution
- potential & physiologically available energy
- alcohol obesity: increases visceral fat
- empty calorie food limit
- try to keep added fat within 32-36% calories
- added sugar: 15-20%
- alcohol: 5-10%
- nutrient dense food: provides a good/fair amount of one or more essential nutrients relative to calorie amount
- multiple causes of hangovers
- substances in alcohol called congeners
- dehydration of brain cells
- health benefits of alcohol
- decreased heart disease risk
- decreased Alzheimer’s risk
- but unmoderated drinking increases many risks (e.g. diabetes, stroke, cancer)
Diet and Cancer
- high intake of fat & alcohol promotes genetically altered cells to cancerous cells → tumor → metastasize to other places
- initiation (DNA error) → promotion (cancer) → progression (metastasis)
- est. 30-60% cancer preventable through diet
- cancer diet risk
- alcohol
- binge drinking: 2 drinks/day dramatically increases cancer risk
- avoid drink & smoke together
- high fat: breast, colon, prostate cancer
- esp. saturated
- salt-cured, char-broiled, pickled, or smoked foods: colon cancer
- naturally occuring mutagens in foods/fruits/veggies (not a big risk)
- additive & pesticides (not a significant risk since they are well-regulated & rinsed before use)
- alcohol
- cancer diet prevention
- fiber: dilute carcinogen and decrease exposure time
- antioxidants: lower risks of all cancer risk (protect cells from oxidative damage and intrusion of carcinogen into cell membrane)
- C, E, beta-carotene (food sources only); supplement can cause negative influences
- phytochemicals: protective factors found in food (purple dyes, beta-carotenes, etc)
- from: blueberries, purple fruits/veggies, yellow fruits/veggies (beta-carotene), green fruits/veggies (green pigment/chlorophyll), red fruits/veggies (lycopene, beta-carotene), orange fruits/veggies (beta-carotene, etc), coffee, chocolate, etc
- carotenoids: alpha-carotene, betacarotene, lutein, lycopene, zeaxanthin, etc
- neutralizes oxidation reactions that damange cellular structure
- lycopene: tomato, watermelon, pink grapefruit
- help males reduce prostate cancer risk
- flavonoids: flavones, flavonols (e.g. quercetin), catechins (e.g. EGCG), anthocyanidins
- soy contains a lot of protective factors (especially isoflavones)
- decrease heart disease
- may contain estrogen-like compound, but does not affect testosterone levels and actually lower prostate cancer risk
- white food: organosulfur compounds: allylic sulfides, indoles isothiocynates
- interfere with cancer growth
- yam, garlic, etc
- cruciferous vegetables: cauliflower, broccoli, kale, etc (leafy greens)
- reduces risks for breast cancer, colon cancer
- a lot of fiber as well (slowly incorporate food to prevent digestive stress)
- cancer risk reduction recommendations
- maintain healthy body composition
- prevent weight gain with age
- eat five or more servings of colorful fruits and vegetables daily
- choose whole-grain foods over refined-grain versions (fiber + phytochemicals)
- limit salt-cured, smoked, pickled, charbroiled foods, and red & processed meat intake
- limit alcohol consumption (note that “saving” the recommended daily intake of 1/2 drink for a single-day binge drinking doesn’t work)
Week 9 - Food Security
Intro to Food Security
- food security: having enough & nutritious food to eat consistently & sanitarily
- food insecurity: limited or uncertain availability/access to nutritious and sanitary food
- food security benefits
nutrient adequacy
- longevity
- food insecurity risks
- nutritional deficiencies
- risks of chronic diseases
- psychosocial effects
- depression, anxiety, embarrassment
- history
- scarcity causes
- drought
- floods
- war
- pests
- diseases (crops/livestock)
- scarcity causes
- pillars of food security worldwide
- availability
- food aid
- food stocks
- domestic production
- import capacity
- accessbility
- purchasing power
- income of population
- transport & market infra
- utilization
- food safety
- diet quality & diversity & meeting needs
- stability
- weather variability
- price fluctuations
- political / economic factors
- availability
- 29% of population is experiencing food insecurity
- food insecurity high risks group
- children (vitamin A / blindness)
- pregnant/lactating individuals (iron)
- elderly (eats less food over time)
- promotion of food security
- UNICEF: health in children
- Kelen Keller Intl: vision-related
- World Food Programme: emergency food aid
- promotion stragies
- cash aid
- food distributions
- micronutrient supplements
- vitamin injections
- food security in US
- components
- quantity
- quality (nutrient density)
- suitability (physical conditions, religious beliefs, etc)
- psychological (sufficient to alleviate anxiety, depression, and monotony)
- social (food is obtain through acceptable ways)
- population survey: over 40M individuals food-insecure (10.5% of households)
- location
- cities & rural have higher food insecurity compared to suburbs
- northeast & south have more food-insecure
- high-risk groups
- elderly (food intake, income)
- women-headed single-parent households (income)
- children (food insecurity have dangerous effects)
- low-income households/individuals
- black & hispanic households/individuals
- COVID had no major change to statistics, but may still have effects on food security
- improvement approaches
- main approaches: food assistance programs, education programs
- Supplemental Nutrition Assistance Program (SNAP)
- CalFresh in CA
- can also provide financial security (money originally budgeted to buy food can be used for rent, etc)
- Special Supplemental Nutrition Assistance Program for Women, Infants, and Children (WIC)
- provides nutritious foods, classes on nutritions, nutrition information, & referrals to health care
- National School Lunch Program (NSLP)
- low-cost / free school lunches
- COVID: free
- movement to extend program to all students regardless of income
- Supplemental Nutrition Assitance Program Education (SNAP-Ed)
- county-by-county basis
- reach low income community & SNAP recipient
- nutrition & physical activity curricula
- improves nutrition behaviors
- Pandemic Electronic Benefits Transfer (P-EBT)
- provides financial assistance for food purchases
- components
- food security in college
- 41% students experience insecurity
- impacts
- physical health
- insufficient sleep (<3d/w)
- increased BMI (33% overweight/obese vs 25%)
- mental health
- academic performance
- lower GPA (-0.17 grade points)
- more likely to consider dropping out (~3.5x more likely)
- neglect academics (>3x more likely)
- physical health
- regional patterns of food insecurity
- southern universities: 13-70%
- western universities: 12-45%
- eastern universities: 12-30%
- high-risk groups
- black/African: 4x
- multiple forms of financial aid: >5x
- housing issues: 8x
- UC food insecurity
- ~40% insecurity
- groups
- Hispanic: 80% more likely than white
- upperclassmen: 3x more likely
- first-gen/transfer: 2x more likely
- basic needs: housing security & transportation > food security
- UC Davis resources
- Aggie Compass
- referral to counseling
- food assistance
- budgeting tools
- emergency & short-term housing assistance
- ASUCD food pantry
- Fruit and Veggie Up!
- Freedge
- Aggie Compass
Week 10 - Nutrition & Athletic Performance
Exercise Fuel Use
Calories burned for one hour of exercise:
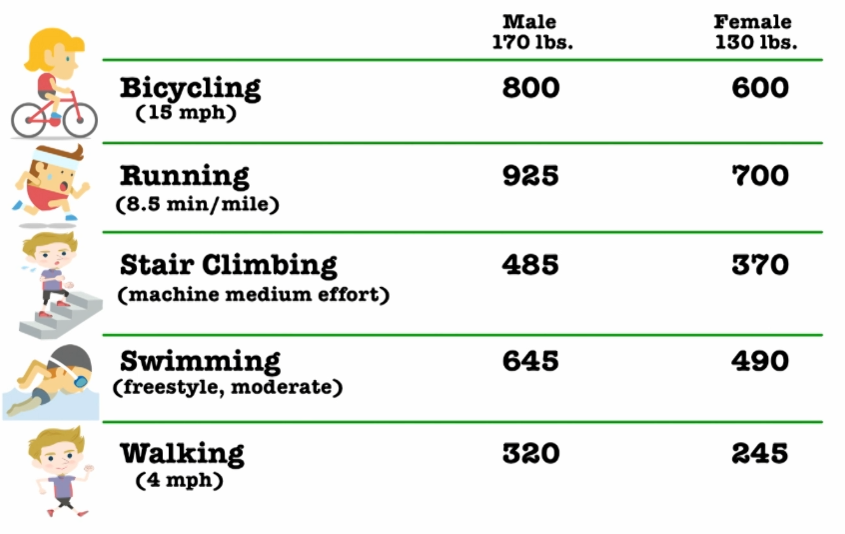
energy source during exercise
- carb: glycogen (limited); can be used for anaerobic
- fat: fat stores (practically unlimited)
- protein: functional tissue (limited; minimal use)
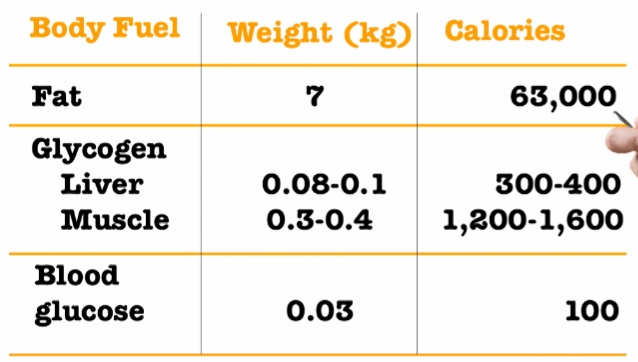
| system / source | used when? | exercise type |
|---|---|---|
| creatine, ATP | < 30s | high intensity/sprint |
| glucose (anaerobic) | 30s ⇐ t ⇐ 2m | high intensity/sprint |
| glucose (aerobic) | 2min - 5h | aerobic (high) |
| fat (aerobic) | 2min - 5h | aerobic (low) |
- high aerobic: basketball, swimming, running, etc (carb used more than fat)
- low aerobic: soccer, cycling, walking, weight-lifting, stretching, etc (fat used more than carb)
fuel use during exercise
- TG in fat cells (50,000-100,000 kcal) → free fatty acid (FFA) in blood
- intramuscular TG (2,000-3,000 kcal) → FFA
- glycogen → glucose
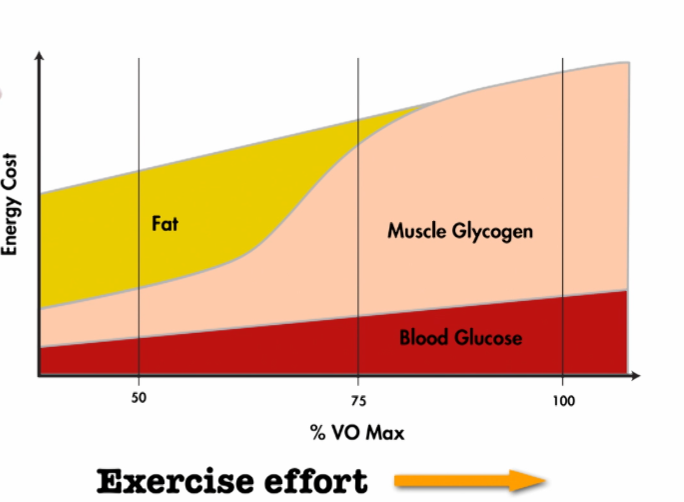
Low intensity exercise doesn’t necessarily burn more fat, because:
- High intensity exercise burns more calories per unit time, making it easier to get a calorie deficit.
- High intensity exercise raises the BMR, which also makes it easier to get a calorie deficit.
Body Energy Stores
Glycogen store gets depleted during long exercises:
.png)
- Better athletes burn more fat so that they can slow down glycogen store depletion (and avoid feeling exhausted).
- Eating more carbohydrates can lead to better endurance during exercise, since there’s more glycogen store.
- increased carb diet for athletes: 450-600 g/day
- increased glycogen store
- prolonged endurance
- improved recovery from endurance exercise
- increased carb diet for athletes: 450-600 g/day
- Carb load before race?
- Don’t do sudden uptake of carbohydrates
- Instead, taper training 1-2 weeks before race and gradually increase carb intake.
Athlete & Protein Intake
- Daily training stresses muscles and causes increase in muscle protein & improved ability to utilize fuel.
- Exercise protein diet: 50-100% above RDA
- 1.2-1.6g protein/kg body mass/day
- used to repair muscle & as a fuel source for endurance training
- muscle building
- eat high quality protein
- after exercise, eat 20-25g protein & 35g carbs to replenish glycogen store
- research shows that foods with leucine (EAA) trigger protein synthesis after exercise
- food sources: lean meat, dairy, whey
- sufficient calories (in >= out)
- consume 30-40g protein one hour prior to sleep (help promote muscle synthesis at night)
- protein powder & drinks?
- convenient
- may offer advantage for recovery from heavy exercise regiments (glycogen & muscle)
- not superior to food
distribution of total calories
| Non-athletes | Athletes | |
|---|---|---|
| Carb | 50-55% | 60-65% |
| Protein | 12-15% | 12-15% |
| Fat | 25-35 | 20-25% |
Water Needs
- Water is an essential nutrient.
- function of water in body
- temperature regulation (release heat through sweat & its evaporation)
- body fluids (blood, lymph)
- transport of nutrients
- waste removal
- water expenditure during exercise: 1-2L water/hour
- trained athletes release more sweat during exercise to maintain body temperature, so they need more water intake
- dehydration
- hydration ~= about 5 full bladders a day
- early warning signs
- fatigue
- loss appetite
- nausea
- poor concentration
- flushed skin, feeling chill (but body temperature does not decrease)
- light-headedness
- dark urine
- pale yellow = hydrated
- yellow/orange = dehydrated
- dark, grayish yellow = severely dehydrated
- muscle cramp (not always)
- muscle cramps
- diet is NOT a direct cause
- mostly caused by fatigue
- some are genetically prone to cramping
- NOT related to potassium
- solution
- drink water
- rest
- hydrate before exercise & when cramp starts
- fluid needs increase with exercise
- 1-2L fluid loss/hr during intense exercise
- drink 2 cups of fluid prior (~30m) to exercise
- drink 1/4-3/4 cup every 15-20 minutes during exercise
- drink beyond thirst post-exercise
- salt loss during exercise; need to replace?
- body store lasts 1-2h, otherwise get it through sport drink, etc
- sport drinks
- consider drinking if exercise is intense or long
- contain 6-9% (by mass) carb
- electrolyte in sports drinks
- maintains body fluid balance
- Na, K, Mg (sometimes)
- replaces electrolytes lost in sweat
- enhances desire to drink it
- better flavor
- coconut water
- intracellular water - high in potassium
- not really that useful as a “sport drink” since potassium is not lost through sweat or during exercise
- fueling before, during, after race
- pre-workout meal
- 2-4h before race
- high in carb: 100-200g
- low fiber: reduce bowel movement
- moderate in protein (15-20g)
- low in fat (fat is slow to digest and is not a limiting fuel since body has plenty)
- limitations for prolonged strenuous exercise
- dehydration
- depletion of muscle glycogen store
- low blood glucose
- exercise refueling (during exercise) strategy: carb + water
- drink 1/4-3/4 cup every 15-20 min during exercise (rule of thumb: every gulp is an ounce)
- consume 30-60g carb every hour, or 100kcal/hr of training if training < 2.5h (60-90g/hr if longer, such as 6-8hrs)
- use water, sports drink, energy bars, carb gel, fruits
- energy bar: pay attention to the target demographic
- carb (often simple + complex)
- avoid fiber (exercise causes lower blood supply to intestine; high fiber may cause distress)
- beware that some energy bar are sold as meal replacement (they will have protein, minerals, vitamins which are not necessary for exercise)
- energy gels: concentrated carb gel of maltodextrin, fructose, dextrose
- easy to carry
- no chewing
- rapid consumption
- carb chews: gummy-like products
- energy bar: pay attention to the target demographic
- sample marathon fueling plan
- mile 6: 8oz sport drink
- mile 12: carb gel
- mile 15: apple slices, 8oz sport drink
- mile 17: carb gel
- mile 21: 8oz sport drink
- total carb: 115g
- post-exercise refueling
- need a lot of carb to replenish glycogen stores
- fluids (16oz for every lbs of sweat loss; measure by weighing on a scale)
- carbohydrate (0.7g/lb body weight; eat within first 30min after exercise)
- protein (20-25g for muscle repair, immune system support)
- antioxidant & other minerals
- example
- tuna sandwich & 8oz cranberry juice (red: rich in antioxidant)
- 2 mozzarella sticks, whole grain English muffin, orange
- fruit smoothie (soy, fruit)
- bean burrito & 6oz juice
- chocolate milk?
- can be superior to some other foods
- protein: 14g/12oz (whey specifically facilitates recovery)
- excellent carb source: 47g
- vit D, calcium, riboflavin @ 20-40% DV
- pre-workout meal
- performance booster (a.k.a. ergogenic aids)
- before taking, evaluate evidence and consider potential consequences
- baking soda
- delay fatigue during exhaustive exercise (of durations within 1-7min) by neutralizing lactic acid in muscle
- drink fluid with baking soda (to prevent explosive diarrhea)
- does not improve endurance
- caffeine: adenosine inhibitor/CNS stimulant
- 45m before exercise - feel better, greater endurance
- dose: 200mg
- burn fat & not use as much carb
- for long distance race, a 30mg dose improvesperformance
- carb loading
- beet root juice
- food source of nitrate
- increases performance (more blood flow & more oxygen delivery)
- dose: 0.5L beet juice necessary
- alternative: powderized beet root juice
- doesn’t really help with endurance races (>10k)
Week 10 - Inflammation & Chronic Disease
- human immunity
- innate: humans are born with builtin immunity mechanisms (e.g. skin, immune system)
- adaptive: develops throughout life (vaccine, exposure to disease, etc)
- passive: temporary (e.g. antibodies in breast milk)
- immune system
- types
- innate: first response
- adaptive: acquired; protects against specific pathogens; known antibodies against specific pathogens are memorized
- white blood cells
- helper T cells: sense infection & activate immune cells
- cytotoxic T cells: fight infections
- B cells: produce antibodies
- memory B cell: memorize antibody that corresponds to specific pathogen
- antibody: proteins that can neutralize antigens (pathogens)
- aka immunoglobins (Ig)
- five different types: IgG, IgA, IgM, IgD, IgE
- e.g. IgE has to do with food and respiratory allergens
- types
- inflammatory response
- def: natural process for healing
- phases
- initial stimulus & local activation of inflammatory factors
- activation of inflammatory pathways
- recruitment of inflammatory cells from blood stream & secondary inflammatory factors are released (can cause pain)
- repair
- activators
- infectious factors: bacteria & viruses
- non-infectious factors: physical wounds, chemicals, damaged cells, psychological factors (stress, excitement), medications, smoking (high oxidative stress), high-fat intake
- types
- acute inflammation: innate immunity
- causes: allergies, injuries, irritants
- chronic inflammation: adaptive immunity (ongoing stimulus)
- acute inflammation failed to handle stimulus
- causes: CVD, pancreatic disease, intestine tract disease, cancer, rheumatoid arthritis, neurological disease, reproductive disorder/disease, lifestyle (smoking, alcohol, too much exercise, stress, high sugar, high fat), etc
- can damage cells
- increases risks of chronic diseases (diabetes, CVD, dementia, depression, cancers) & risks of mortality (old individuals)
- acute inflammation: innate immunity
- food allergy vs food intolerance
- food allergy
- affects immune system
- severe to life-threatening
- small amounts to trigger
- food intolerance
- affects digestive system
- less serious
- may tolerate small amounts
- possible causes
- enzyme deficiencies
- sensitivity to additives
- reactions to naturally occuring chemicals in food
- food allergy
- Which are inflammation causes?
- dairy: inconclusive
- fermented diary could be anti-inflammatory (not conclusive)
- allergy
- reaction to diary proteins
- severity ranges from rashes to anaphylaxis
- symptoms may overlap with lactose intolerance, but allergy also affects other areas
- antihistamine can help with mild allergy
- added sugar: linked to inflammation in animals, inconclusive results in human trials
- cognitive impairments
- linked to increased risks of CVD, cancers, excess body fat + type 2 diabetes (low-grade chronic inflammation), non-alcoholic fatty liver disease, arthritis, gut permeability (leaky gut), increased LDL, etc
- free fructose (added): linked to fatty liver
- increased in liver fat
- may cause steatosis hepatitis (nonalcoholic fatty liver disease)
- gluten: linked to inflammation (in presense of celiac disease & NCGS)
- protein found in wheat, rye, & barley
- only need to avoid if has celiac disease & NCGS
- uncertain results of gluten’s effect on general population
- wheat allergy: IgE-mediated reaction to gliadin protein
- symptoms: itching, swelling, skin, rash, anaphylaxis (life-threatening)
- symptoms take minutes to hours
- fat: high fat diet linked to inflammation in human trials
- reduce to below 35% calorie intake
- low-grade systematic inflammation
- change homeostasis in many organs
- type, source, amount of fat all matter
- saturated fat (solid fat): <10% total calories
- Omega-3
- reduces risks of CVD by reducing inflammation
- DHA better than EPA
- dairy: inconclusive
- chronic diseases: conditions that last 1 year or more, requires ongoing medical attention or limit activities of daily living, or both
- 41 million of deaths per year = 71% of death
- examples: heart disease, cancer, chronic lung disease, stroke, Alzheimer’s disease, diabetes, chronic kidney disease
- connection to inflammation
- chronic low-grade inflammation linked to cancer, type 2 diabetes, neurodegenerative diseases, CVD
- lowering inflammation may reduce risks of many chronic diseases
- ”anti-inflammatory diets” (Tom Brady)
- not evidence-based
- don’t follow the trend
- Mediterranean diet
- food to reduce inflammation
- habits that may reduce inflammation: meditation, walks, journaling, adequate sleep
Week 10 - Dietary Guidelines
- good protein sources
- lean cuts of beef, pork, poultry,
